SCENE
A BP Canada filling station on Lakeshore Blvd. in Etobicoke, On. Canada.
INCIDENT HISTORY
10:25 am/Monday: 33-year-old Rochelle was fueling her 2011 Chevy Malibu at a BP Canada filling station when a 2007 Camaro plunged into Rochelle’s fuel dispenser. The Camaro also sideswiped a car pulling out of another fuel dispenser. Its front airbags deployed as Rochelle’s fuel dispenser shattered to the ground. Reacting quickly, she dropped her fuel pump and fled. As she did, her fuel dispenser caught on fire. As the flames spread to the Camaro’s engine, she saw the driver slumped in his seat. Realizing he was unconscious in a car about to explode, she hurried over to get him out as quickly as possible.
Startled, Rochelle could not gather her thoughts. Startled, Rochelle could not collect her reviews. Rochelle flung open his driver-side door, unfastened his seat belt, pulled him out of the car, and dragged him away. Seconds later, the fuel dispenser, the Camaro, and Rochelle’s Malibu exploded. A passerby rushed to help as she pulled the unconscious man away from the crash scene. The passerby called 911 to request urgent medical assistance for Rochelle and the unconscious driver. He explained that the entire gas station would go ablaze, requesting police, fire, and paramedic assistance. The big booms and blazing fire attracted the attention of many others.
A man was dragged from the wreckage by a customer who was fueling her car
at the time of the accident.”
CALL INFORMATION
Etobicoke Paramedics received a code 4 for an MVC (motor vehicle collision) at a BP Canada station on Lakeshore Blvd. It involves a crash at the fuel dispenser. Arriving in five minutes, they found a noticeably rattled Rochelle and bystanders. Someone fueling her car at the time of the accident dragged an unconscious man from the wreckage. An unconscious male lies on the ground a hundred feet from the two-car inferno. A crowd of onlookers watched, and CP24 News was also on the scene. They informed the medics that there were several explosions. The patient may have smoke inhalation and burns.
INCIDENT HISTORY cont…
Upon contact, the patient’s eyes were closed while he responded to voice and stimuli (AVPU). He mumbled some words about chest tightness and sharp pains in his left arm. As firefighters extinguished the blaze, paramedics wore personal protective equipment (gloves, mask, and goggles). His Glasgow coma scale was 8. Allied assistance (police and fire) were on the scene (P-EMCA). The environment was relatively safe; there were two casualties, Rochelle and the semi-conscious male; the mechanism of injury was a semi-conscious male who may have smoke inhalation and burns and a female who was startled.
Calling for an additional unit, a paramedic determined with a primary assessment that Rochelle showed no signs of trauma, pain, bleeding, or infection. She gave her 15 liters of oxygen on a non-rebreather mask and advised her to see a physician. The paramedic released Rochelle to the police. The other medic asked his partner, who was through with Rochelle, to hold C-Spine as he confirmed the patient’s fully present, equal, and matching carotid and radial pulse. He noticed first-degree burns on his face (9% using the rule of nines). His airway was clear, with no angioedema, but his breath gave off a sweet smell.
He noticed first degree burns on his face (9% using the rule of nines). His airway was clear with no angioedema found but his breath gave off a sweet smell.”
His breathing was Kussmaul at 42 breaths a minute (CAB). The medic put a dry sterile dressing between the mask and the first-degree burn on the patient’s face and gave him 15 liters of humidified oxygen on a non-rebreather cover. He palpated his cervical vertebrae for crepitus, deformities, step-offs, and abnormalities; none were found. C-spine could not be ruled out, so a collar was administered. They inspected his head for contusions, lacerations, abrasions, and puncture or swelling (CLAPS) and felt for tenderness, instability, crepitus, and swelling (TICS), but none were found.
There was no rhinorrhea, otorrhea, cerebrospinal fluid (CSF), mastoid bruising, or jugular vein distention. His trachea was in its normal anatomy showing no signs of pneumothorax. The patient’s breathing was not flailed. Preparing to backboard him, vital signs were taken (see below), and his clavicle, chest, sternum, and ribs were inspected for CLAPS and palpated for TICS. His upper right left, lower right, and left abdominal quadrants were palpated for anomalies, but none were found. First-degree burns were found on his chest (18%), with second-degree burns on his right arm (9%).
A woman identifying herself as the patient’s mother arrived on the scene. She divulged his name and explained that he is a type one diabetic who may have forgotten to take his insulin after he found out his wife was divorcing him for the cable guy. From this information, the paramedics presumed that his mechanism of injury should be upgraded to diabetic ketoacidosis with first and second-degree burns to his face, arms, and chest. Paramedics immediately administered insulin to the patient. The dry sterile dressing was applied to the first-degree burns on his chest, and a moist sterile dressing was used for the second-degree burnt region on his right arm. The arm was then placed in a sling. The patient was dosing in and out of consciousness.
She divulge his name and explained that he is a type one diabetic who may have forgotten to taken his insulin after he found out his wife was…”
The medic pressed in, pulled out, and pushed down on Steinberger’s pelvis to ascertain dislocation, fracture, or internal bleeding; none were found. The opposing force was applied on both his thighs to confirm a femur fracture or internal bleeding; none were found. The paramedic asked his partner (holding C-spine) to count to three as they turned the patient on his side to inspect his back, thoracic, and lumbar vertebrae for CLAPS and TICS; none were found.
They applied cervical safeguard, back boarded him, loaded him on the stretcher, and took his second vital signs. The patient was then auscultated with 4 points, apex to base bilaterally. No adventitious sounds were heard. There were no penetrating wounds, only a slightly pale skin discoloration. A gross wet check found no external bleeding, medical bracelets, or alerts.
They boarded the ambulance.
CHIEF COMPLAINT
Steinberger’s chief complaint was burned. She had just run and dragged a 250 lbs male from a burning car. She was not hit by debris, did not inhale anything, nor was she injured. The chief complaint from Rochelle was that she was breathing fast because she was startled by the ordeal.
Upon contact with him, paramedics did not know he was a type one diabetic. Hence, they were more concerned about a possible fracture, smoke inhalation, spinal cord injury, and pneumothorax from an impaled object. His Kussmaul breathing made them assume he was hypoglycemic until his mother confirmed he was a type one diabetic who took insulin.
VITAL SIGNS
| FIRST VITAL SIGNS | SECOND VITAL SIGNS | THIRD VITAL SIGNS |
| BP – 168/100 – Flushed skin | BP – 132/86 – Skin – pink | BP – 124/52 – Skin – pink |
| Temp – 98.0 | Temp – 98.4 | Temp – 98.0 |
| Pulse – 92 Full | Pulse – 86 Full | Pulse – 70 Full |
| Resp. – 42 Full | Resp. – 30 Full | Resp. – 24 Full |
| SP02 – 89% | SP02 – 94% | SPO2 -96% |
| Glasgow Coma Scale – 8 | Glasgow Coma Scale – 10 | Glasgow Coma Scale – 10 |
| Pupils – 3mm round/matching | Pupils – 6mm round/matching | Pupils – 6mm round/matching |
PATHOLOGY
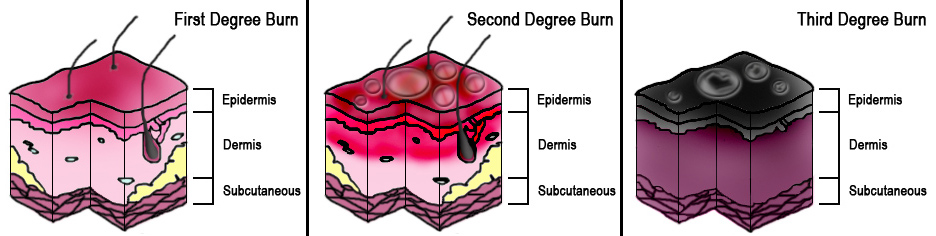
Burns: Thermal burns occur when skin is exposed to temperatures above 44 degrees centigrade. The severity of thermal injury correlates directly with temperature, concentration, or amount of heat energy the object or substance possesses and the duration of exposure. Superficial burns involve the epidermis only with skin redness and swelling. Partial thickness burns involve the epidermis and varying degrees of the dermis with pain and blistering.
Full-thickness burns involve the destruction of both layers, including the basement membrane of the dermis, thus making it incapable of self-regeneration. Full-thickness burns are painless and have a waxy appearance. The total body surface area burned is calculated using the rule of nines. Others are the rule of palms and Lund and Browder chart. Burn shock is a result of hypovolemia caused by fluid shifts. GBurn shock is a result of hypovolemia caused by fluid shifts. Fluid resuscitation is essential Burn shock results from hypovolemia caused by fluid changes. UUBurn shock results from hypovolemia caused by fluid shifts ring the first 24 hours to prevent burn shock.
Upon contact with him paramedics did not know yet that he was a type one diabetic
so they were more concerned about a possible fracture, smoke inhalation, spinal cord injury and/or pneumothorax from an impaled object.”
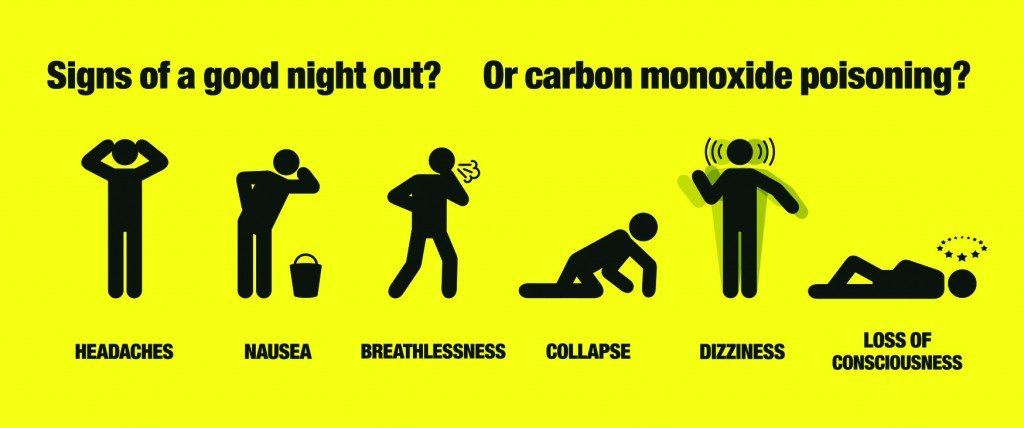
Carbon Monoxide Poisoning: Carbon monoxide has no smell, taste, or color. Its effects are silently poisonous. Carbon monoxide is a by-product of burning natural gas, gasoline, propane, wood, or coal. In the case of fire, it is a likely cause of death. Its hazard is expanded when that incineration is in a closed environment. It also builds to hazardous levels from the exhaust of generators, heaters, barbecue grills, or other appliances in well-ventilated spaces.
CO is particularly dangerous since there are no obvious signs of its initial build-up in the air. It can prevent oxygen from bonding with hemoglobin in the blood during perfusion. This can cause hypoxia and hypoxemia. Since our patient was unconscious, it was easy to assume he had carbon monoxide poisoning. In his case, it was ruled out because he did not complain of a headache, was not exhausted with shortness of breath, or impaired his motor functions.
He had Kussmaul breathing. He complained of tightness in the chest instead of chest pain and did not convulse. He did not throw up, either. So this condition was not applicable.
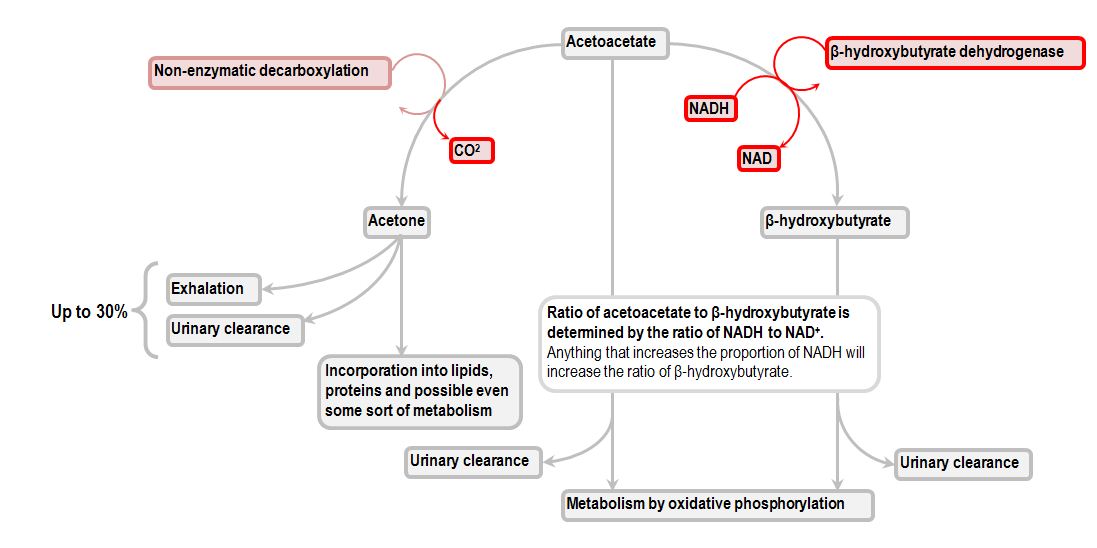
Diabetic Ketoacidosis: The human body needs energy to function. Cells metabolize glucose to produce energy. For glucose to enter a cell, it requires insulin to admit its entry. Once inside the cell, glucose undertakes glycolysis, transforming it into pyruvate. Pyruvate enters the cell’s mitochondria and launches a curb cycle to become ATP (adenosine triphosphate).
ATP is the body’s primary source of energy. Without glucose, tissues such as the heart, brain, kidneys, or liver starve for fuel. Insulin is also needed within the cell to inhibit fatty acids from being transported to the matrix of the mitochondria to take part in glycolysis and the Krebs cycle.
The body’s cells metabolize fatty acids to create energy since there is no insulin to admit glucose into the cell. When there is no insulin, glucose remains in the bloodstream. This leads to hyperglycemia (too much glucose in the bloodstream). The kidneys will flush out excess glucose by causing thirst and frequent urination. Hyperglycemia can be seen in people who have not eaten in hours (fasting hyperglycemia) or those who have eaten within the hour (postprandial hyperglycemia). Whatever the case, polydipsia, polyuria, and polyphagia become present.
The LB hydroxyacyl CoA is dehydrogenated again to create B ketoacyl CoA through B hydroxyacyl CoA dehydrogenase.”
This is done by beta-oxidation, where chains of fatty acids go through dehydrogenation to create a paired link of C2 and C3. The resulting acyl-CoA produces a trans two enoyl-CoA delta. Trans 2 delta enoyl-CoA is then hydrated at the paired bond to produce LB hydroxy acyl-CoA. The LB hydroxy acyl CoA is dehydrogenated again to create B ketoacyl-CoA through B-hydroxy acyl-CoA dehydrogenase.
NADH is used as an electron acceptor, and thiolysis occurs between C2 and C3 (alpha and beta carbons) to produce B ketoacyl-CoA. Thiolase enzyme catalyzes the reaction wherein new molecules of coenzyme A break the bond by nucleophilic attack on C3. This discharges the first two carbon units, acetyl-CoA and a fatty acyl-CoA minus two carbons. This process will repeat itself until all carbons in the fatty acid are turned into acetyl-CoA, and ketone bodies are produced. Those ketones can then be used as substitutes for ATP, providing energy to the body.
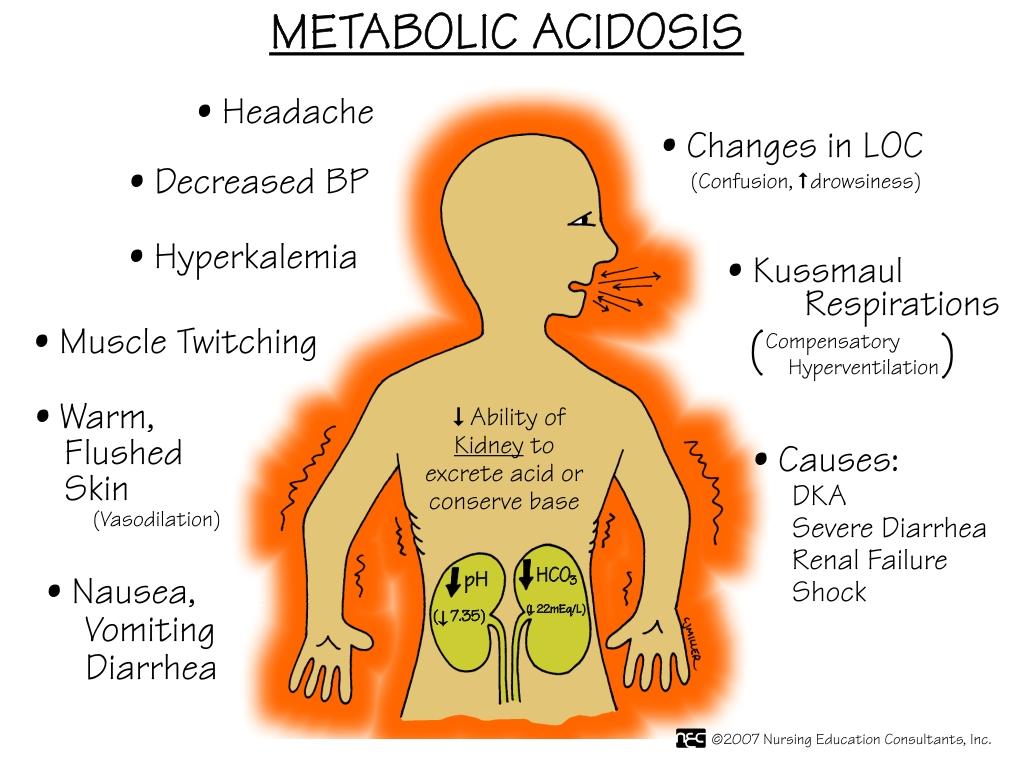
Ketone bodies are acidic and high in potassium. When Ketone bodies migrate from the cell in diabetic ketoacidosis, they ooze into the bloodstream. The kidneys recognize the imbalance and excess of glucose and ketones in the bloodstream. This causes them to trigger an osmotic diuresis of the excess water, drunk due to polydipsia, to flush out the excess glucose and ketone bodies through urination. Osmotic diuresis leads to dehydration.
With a system high in glucose and imbalanced amounts of ketones, the kidney works overtime to expel the excess glucose and ketone bodies high in potassium. Expulsing that much potassium too fast can prompt the heart to malfunction. The increase of ketone bodies in the bloodstream also causes a drop in the PH level.
They concluded that Steinberger blacked out behind the wheel due to a diabetic shock.”
In Steinberger’s case, paramedics affirmed that he was suffering from dehydration, metabolic acidosis, depletion of potassium, and a lack of insulin with excess glucose and ketone bodies. They also suspected ischemia. The Kussmaul breathing was his lung’s attempt to rid his blood of its excess carbon dioxide and waste products from beta-oxidation.
They concluded Steinberger blacked out behind the wheel due to a diabetic shock. They resolved that he was burned while passed out in the car and did not suffer carbon monoxide poisoning because Rochelle pulled him out. Had he stayed in the car, he would also have had more severe burns.
SIGNS AND SYMPTOMS
Burns: With superficial burns, the skin is red and swollen. When touched, the color will blanch and return. Patient experience pain because nerve endings are exposed to the air. Partial-thickness burns are more painful than blisters. A full-thickness burn appears white and waxy brown and leathery or charred. Inhalation burns and intoxication is significant problems that may cause angioedema and block airways.
There may be a headache, dizziness, shortness of breath, and irritation of eyes, nose, throat, and chest hence assess for signs of inhalation such as smoky breath odor, burns to lips, carbon particles in saliva, crackles on chest auscultation and decreased air entry.
Carbon Monoxide Poisoning: The patient did not complain of a headache. The patient was not fatigued with shortness of breath or impaired motor functions. He had Kussmaul breathing. The patient complained of tightness in the chest instead of chest pain. He did not convulse. His unconscious state was due to acidosis from a lack of insulin.
Diabetic Ketoacidosis: The patient’s Kussmaul breathing was a leading indication. His acetone breath signaled that he was acidotic. Acidity triggered hyperventilation as his lungs rid his body of excess carbon monoxide. His skin was flushed, he was unconscious, had hyperthermia, and had urinated. Since he had not taken his insulin, he was having diabetes mellitus as well as osmotic diuresis. It was deemed that low potassium from osmotic diuresis could also make him hypokalemic and trigger a cardiac arrest.
INCIDENT HISTORY cont…
En route to the closest hospital, paramedics noticed the patient’s condition had improved. He was incontinent of urine at the scene, but now his consciousness was improving. Since they administered his insulin, his breathing was slowly becoming normal. He was now partially awake. He explained that the tightness in his chest and pain in his left arm was gone, but he needed to urinate. The patient was asked:
The onset of the event: As he drove to work, he felt some tightness in his chest and thought it was stress. He said he started hyperventilating once he pulled into the BP Canada filling station and does not remember what happened afterward.
Provocation or palliation: The patient said he was on his way to work. He argued with his wife earlier. She informed him their marriage was over. She’d been seeing the cable guy. He was upset. He stormed out and forgot to take his insulin. He was too upset.
As he drove to work he realized he needed to buy gas so he pulled into the BP Canada station.”
The quality of the pain: The patient said there was a throbbing pain in his left arm, but it’s gone.
Region and Radiation: The pain was only in his left arm; It did not radiate to his chest, jaw, or other body parts.
Severity: The patient explained that when the pain was at its worst on a scale of 10, it was 4.
Time (History): The patient said he was fine until the argument. Once they argued, he felt slightly panicky on his way to work. He did not remember to take his insulin. As he drove to work h,e realized he needed to buy gas s,o he pulled into the BP Canada station. As he did, he began hyperventilating and felt chest tightness with pain in his left arm. He soon felt lightheaded and dodidn’temember what happened afterward.
BLS TREATMENT
Burns:
Stop the burning process by using dry sterile dressing on his face, which had first-degree burns, and a moist dressing was applied to the chest and right arm, where he had second-degree burns.
They performed a rapid trauma assessment.”
Administer high-concentration humidified oxygen. In the case of facial burns like in this case, gauze pads are placed on the edges of the oxygen mask to decrease pain and irritation.
Cover with wet sterile dressings for 1st and 2nd-degree burns <10 -15%; cover more extensive 2nd-degree burns and all 3rd-degree burns with a dry clean sheet or bandage.
Elevate the affected part.
Leave blisters intact and dress digits individually.
Cover affected eyes with moist dressings.
Initiate rapid transport if indicated.
Enroute monitor, re-evaluate and manage as required for concurrent injuries
i) emesis
ii) seizures, combative behavior, the decline in the level of consciousness
iii) hypotension, shock
iv) airway obstruction and distress
Diabetic Ketoacidosis:
Paramedics assumed the patient was hypoglycemic when informed that he had diabetes.
They performed a primary assessment of the patient. Due to the MVC, the call was now a trauma even though the patient only showed signs of medical issues. They performed a rapid trauma assessment. They initiated cardiac monitoring (the patient’s pulse rate normalized after his insulin was administered). They performed his blood sugar glucometer.
Vital signs included:
Three different vital signs were taken. Skin assessment of his color, condition, and state of dehydration. Mouth, in which his airway, breath odor, and state of dehydration. The central nervous system, in which the patient’s pupils were assessed, and his Glasgow Coma Scale was evaluated along with sensory-motor functions.
Carbon Monoxide Poisoning:
Paramedics were told during the call that the patient could be a case of potential carbon monoxide poisoning since he was in a burning car. However, upon assessment, he showed no signs of having been poisoned. There were no signs that he was under the influence of drugs or alcohol. The patient showed no signs of self-infliction or bodily harm.
A head-to-toe rapid trauma assessment was done and redone periodically. Only his Glasgow Coma Scale improved from 8 to 10. His papillary size was equal, and his reactivity was typical.
The patient’s skin color was getting normal. Three full vital signs were collected.
CRITICAL ERRORS/FLAGS
Cooling, extensive burns with dressing may cause shivering and hypotension; thus, a wet dressing is covered with a dry sauce to prevent heat loss.
Delay in fluid resuscitation may lead to burning shock.
SAMPLE
Signs and Symptoms – Burns on the face, hand, and chest. Unconsciousness, Kussmaul breathing, acetone breath smell, chest tightness, and redness of the face, chest, and arm.
Allergies – None
Medications – Lipitor, insulin
Past Medical History – Type one diabetes
The last Intake – Took insulin the previous night.
Events Leading Up to the Incident – The patient was in a heated argument with his wife when she told him she was already talking to divorce lawyers. He stormed out of the house without taking his medications. While driving into a BP Canada gas station, he became unconscious. The patient does not remember what happened next. He was going in and out of consciousness when paramedics arrived.*
REFERENCES
Nancy Caroline’s Emergency Care on the Streets
Basic Life Support
Patient Care Standards